4 Common Factors That May Contribute to Unexplained Infertility
Unexplained infertility can be one of the most frustrating and emotionally exhausting diagnoses to receive. After months or years of trying, being told there is “no clear cause” can feel dismissive or hopeless. But an unexplained infertility diagnosis does not mean there is no reason for difficulty conceiving. It often means that standard testing hasn’t captured the full picture.
For many couples with unexplained infertility, contributing factors exist beneath the surface. Fertility is complex, timing-sensitive, and deeply connected to hormonal balance, inflammation, stress, and overall health. With the right perspective and support, pregnancy success is still very possible.
Below, we’ll explore four common factors that may contribute to unexplained infertility, why this diagnosis is more common than you think, and what options exist moving forward.
What Does an Unexplained Infertility Diagnosis Mean?
Unexplained infertility is typically diagnosed after standard fertility testing shows no obvious abnormalities. This usually includes confirming ovulation, evaluating fallopian tube patency, and performing a semen analysis. When these results appear “normal,” a fertility specialist may label the situation as unexplained infertility.
This diagnosis does not mean pregnancy is impossible or that treatment won’t work. In reproductive medicine, unexplained infertility simply reflects the current limits of testing and not the limits of your body’s potential for pregnancy.
Why Unexplained Infertility Is More Common Than You Think
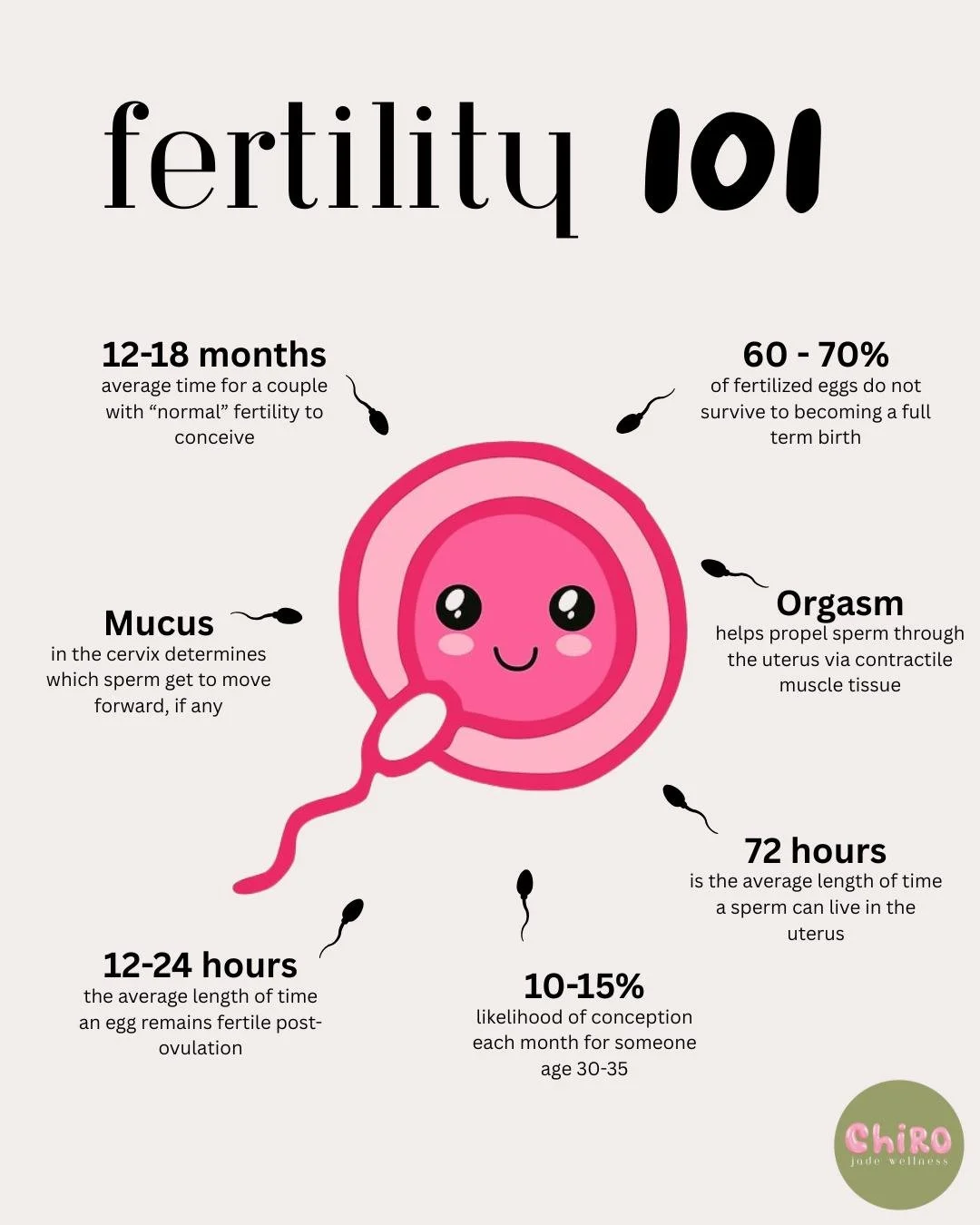
Conception depends on many variables happening at exactly the right time: egg quality, sperm function, hormonal signaling, implantation, and uterine receptivity. While infertility treatment has advanced significantly, not every factor can be easily measured or captured in a single cycle of testing.
Clinical pregnancy rates and cumulative pregnancy rates show that many people with unexplained infertility eventually conceive, either spontaneously or with support. In many cases, treatment improves pregnancy success not by “fixing” a single problem, but by optimizing timing and reducing hidden barriers.
4 Common Factors That May Contribute to Unexplained Infertility
1. Long-Term Hormonal Birth Control and Cycle Disruption
Long-term use of hormonal birth control suppresses natural ovulation by replacing the body’s own estrogen and progesterone with synthetic hormones. While effective for pregnancy prevention, extended use can disrupt the menstrual cycle long after discontinuation.
Some people experience irregular cycles, multiple periods per month, or absent periods for months after stopping oral medications. During post-pill recovery, ovulation may be inconsistent, timing may be unpredictable, and egg quality may be temporarily affected.
Because birth control history is not always emphasized in fertility evaluations, ovulation induction may be recommended when cycles struggle to normalize. Supporting cycle recovery can be a critical step before or alongside infertility treatment.
2. Chronic Inflammation and Implantation Challenges
Inflammation plays a significant role in fertility, particularly in ovulation and implantation. Chronic inflammation—whether from food sensitivities, environmental exposures, autoimmune conditions, or early-stage endometriosis—can interfere with hormonal signaling and uterine receptivity.
Even when imaging or labs appear normal, inflammation can disrupt the luteal phase and lower ongoing pregnancy rates by creating a hostile uterine environment. Addressing inflammation is often an overlooked but important component of infertility treatment and reproductive technologies.
3. Hormonal Imbalances Not Captured by Standard Testing
Hormonal imbalances such as elevated androgens are commonly associated with conditions like PCOS, but subtle imbalances may go undetected with single-point testing. Hormone levels fluctuate throughout the menstrual cycle, and values that fall within “normal” ranges may still be problematic for an individual.
When hormone imbalance is suspected despite normal labs, fertility treatment options such as ovarian stimulation may be used to support ovulation and improve conception timing. Individualized evaluation is often key when standard testing doesn’t tell the full story.
4. Chronic Stress and Nervous System Dysregulation
Chronic stress has a direct impact on fertility. Ongoing stress elevates cortisol, which suppresses ovulation and signals to the body that it is not a safe time to reproduce. If the nervous system is struggling to return to a rest-or-digest state due to long-term or chronic high levels of stress, ovulation, implantation and even ability to maintain a pregnancy could be affected.
When the body remains in a fight-or-flight state, reproductive hormones are deprioritized. Over time, this can delay conception, extend infertility duration, and reduce pregnancy success even when regular fertility testing appears normal.
Nervous-system-focused chiropractic care can support this process by helping the body more consistently access states of regulation and safety. Gentle chiropractic adjustments work with the brain–body connection to reduce stress signaling, improve communication between the nervous and hormonal systems, and support the body in shifting out of chronic survival mode. For many people navigating fertility challenges, chiropractic care becomes a grounding, stabilizing support that complements fertility coaching and medical care—helping the body feel safer, more regulated, and better resourced throughout the journey.
What Standard Fertility Testing May Miss
Standard fertility testing often focuses on structural and baseline measurements but may miss functional issues. Semen analysis evaluates sperm count and motility, but not always sperm function. Uterine receptivity, subtle implantation barriers, and precise timing challenges are also difficult to fully assess.
Unexplained infertility may involve male factor infertility even when semen analysis results are considered normal. Assisted reproductive technologies are often designed to bypass these limitations.
Fertility Treatment Options for Unexplained Infertility
Intrauterine Insemination (IUI) as a First-Line Treatment
Intrauterine insemination (IUI) is often considered a first line treatment for unexplained infertility. IUI involves placing sperm directly into the uterus during ovulation, improving timing and sperm-egg interaction.
This approach can be paired with ovulation induction medications and is less invasive than IVF. While IUI slightly increases the chance of multiple pregnancies, it remains a common early intervention in fertility treatment.
IVF and Advanced Reproductive Technologies
In vitro fertilization (IVF) allows fertilization to occur outside the body, improving control over egg and sperm interaction and embryo development. IVF treatment can address challenges related to egg quality, sperm function, and implantation.
When male factor infertility is suspected, intracytoplasmic sperm injection (ICSI) may be used to inject a single sperm directly into the egg. These assisted reproductive technologies have helped many couples achieve successful pregnancies after unexplained infertility.
Expectant Management and When Waiting Makes Sense
Expectant management refers to continuing to try naturally without immediate intervention. This approach may be appropriate for some couples depending on age, advanced maternal age considerations, infertility duration, and overall health.
A fertility specialist can help determine whether waiting is reasonable or whether treatment may improve outcomes.
When to Seek Additional Support
If you have been trying to conceive for 12 months under age 35—or 9 months over age 35—it may be time to seek guidance from a fertility specialist. Unexplained infertility can often be treated successfully with the right combination of evaluation, support, and care.
Reproductive medicine offers many pathways forward, and you deserve reassurance and clarity in the process.
How Holistic Fertility Coaching Can Support Unexplained Infertility
When everything looks “normal” on paper but pregnancy still isn’t happening, holistic fertility coaching helps fill in the gaps. This approach looks beyond isolated test results and focuses on how your whole body is functioning—your cycle patterns, nervous system regulation, lifestyle factors, stress load, and subtle hormonal trends that are easy to miss in short medical appointments.
Through one-on-one coaching, we take a personalized, supportive approach to understanding your fertility story. This always starts with reviewing labs and cycle data through a comprehensive, full-cycle blood panel which helps identify patterns that could be impacting ovulation or implantation. We work together to support nervous system regulation and create sustainable shifts that help your body feel safer and more supported during this process. Coaching is not about doing more—it’s about doing what’s right for your body.
Holistic fertility coaching can be especially helpful for those navigating unexplained infertility, repeated disappointment, or feeling stuck between “everything is fine” and “why isn’t this working?” If you’re unsure what your next step should be, I offer a free consultation to explore whether fertility coaching is a good fit for you. This is a no-pressure space to ask questions, share your goals, and decide if this kind of support feels aligned.
You Are Not Alone in an Unexplained Infertility Diagnosis
Many couples with unexplained infertility go on to experience pregnancy success, with or without medical intervention. This diagnosis is not the end of the story—it is simply a starting point for deeper understanding.
With the right support, unexplained infertility can be treated, and hope can be restored. Dr. Savannah offers free consultations to determine if Holistic Fertility Coaching is right for your fertility journey.
-Dr. Savannah
FAQs About Unexplained Infertility
What does unexplained infertility mean?
Unexplained infertility means that standard fertility testing has not identified a clear cause for difficulty conceiving. It does not mean there is no cause—only that it has not yet been identified.
Can unexplained infertility still be treated?
Yes. Many couples with unexplained infertility achieve pregnancy through fertility treatment, lifestyle support, or expectant management. Treatment often improves timing and overall pregnancy success.
How common is unexplained infertility?
Unexplained infertility accounts for approximately 10–30% of infertility diagnoses, making it one of the most common categories seen in reproductive medicine.
Is IVF necessary for unexplained infertility?
IVF is not always necessary. Many people try ovulation induction or intrauterine insemination (IUI) first. IVF may be recommended based on age, infertility duration, or prior treatment outcomes.
How long should couples try before seeking treatment?
Couples under 35 are typically advised to seek help after 12 months of trying, while those over 35 should consider evaluation after 9 months.
Can unexplained infertility resolve on its own?
Yes. Some couples conceive naturally over time, particularly with expectant management. Others benefit from targeted support or treatment.
Does unexplained infertility mean something was missed?
Sometimes. Fertility testing has limitations, and unexplained infertility may reflect subtle factors not easily measured.
When should I see a fertility specialist?
If you have concerns about fertility, prolonged infertility duration, or want guidance on next steps, seeing a fertility specialist can provide clarity, reassurance, and options.