The Guide To Hypermobility for the Newly Diagnosed
Receiving a diagnosis related to hypermobility can feel validating, confusing, and overwhelming all at once. Many people spend years being told their pain is “normal,” that they’re just flexible, or that anxiety is the root cause—only to finally learn there’s a real connective tissue difference at play. Whether you’ve been diagnosed with Hypermobility Spectrum Disorder (HSD) or hypermobile Ehlers Danlos (hEDS), this guide is here to help you understand what’s happening in your body and how to move forward with confidence and support.
This article walks through diagnosis, care options, hypermobility management, trusted hypermobility resources, and how chiropractic care can be adapted safely and effectively for hypermobile bodies.
What is Hypermobility Spectrum Disorder?
Hypermobility Spectrum Disorder is a condition where joints move beyond their typical range due to differences in connective tissue. While many people were told their whole lives they were “double-jointed,” HSD often comes with symptoms such as chronic pain, joint instability, frequent injuries, fatigue, and nervous system dysregulation. And as it would turn out: double jointed simply is not a diagnosis or a real description of what is really happening in a hypermobile body.
Hypermobility exists on a spectrum. Some people experience minimal symptoms, while others deal with widespread pain, proprioceptive challenges, and difficulty recovering from daily activities. Importantly, hypermobility is not just about joints—it can affect fascia, muscles, and the nervous system, which is why a whole-body approach to hypermobility management is essential. It is also why it is imperative that hypermobile people have care provider who are knowledgeable and confident in how this changes their practice.
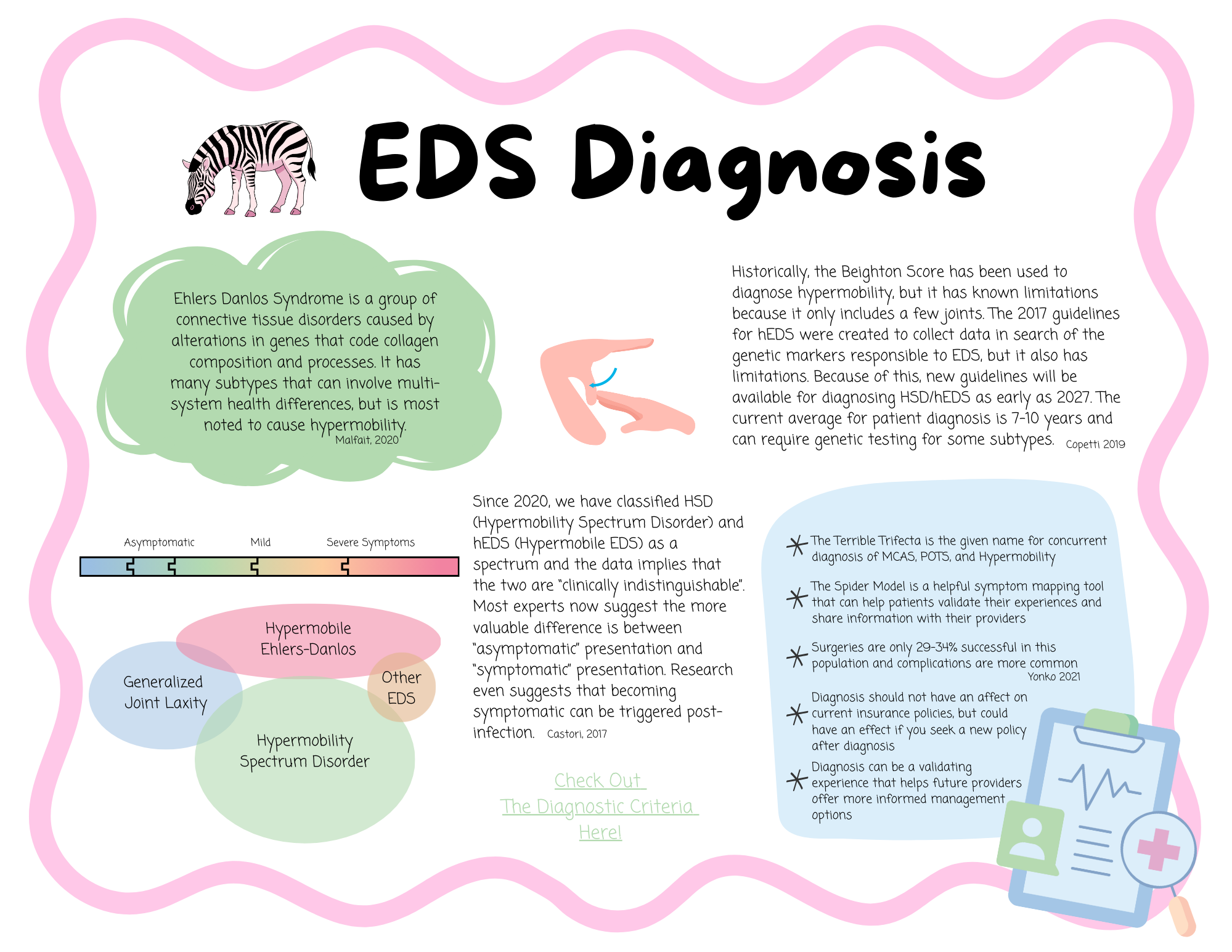
How does diagnosis of HSD and hEDS work?
Diagnosis for hypermobility-related conditions is primarily clinical. Providers assess joint range of motion (often using the Beighton score), symptom history, family history, and how hypermobility affects daily life. There is currently no single lab test that diagnoses HSD or hypermobile Ehlers Danlos, but genetic testing is available for many other types of Ehlers-Danlos Syndrome and may even be covered by your insurance.
Many patients are diagnosed by rheumatologists, geneticists, or knowledgeable primary care providers. Unfortunately, access to informed clinicians can be limited, which is why education and hypermobility resources are so important during the diagnostic process.
Is there a difference between HSD and hEDS?
While there may be a genetic difference between HSD and the subtypes of EDS, they can be clinically indistinguishable. Ehlers Danlos, specifically hypermobile Ehlers Danlos, is a genetic connective tissue disorder with systemic features. HSD is currently diagnosed when someone has symptomatic hypermobility but does not meet the full criteria for hEDS. As of the writing of this article in 2026, the Ehlers Danlos Society is expecting the diagnostic criteria to be updated and the Beighton Scale to be expanded to include other joints by the end of 2027 which could dramatically shift what we currently consider the difference between these two diagnoses. They make note in their trainings that the difference between the two may be more well described as HSD being “asymptomatic” and hEDS being “symptomatic”.
From a care perspective, many management strategies overlap. Both benefit from thoughtful hypermobility management, nervous system regulation, and movement-based support. The label matters less than receiving care that respects your body’s needs.
Resources for Hypermobile Patients
Finding trustworthy hypermobility resources can make a huge difference in how supported you feel. Look for organizations, providers, and educators who specialize in hypermobility and Ehlers Danlos, not just general pain care.
Helpful hypermobility resources often include:
Patient advocacy organizations focused on ehlers danlos
Provider directories for hypermobility-aware clinicians
Educational platforms that explain pacing, stabilization, and nervous system care
Building a care team that understands hypermobility is one of the most empowering steps you can take. You can click here to view a list of resources that has been put together in our office that includes a variety of options available online.
Research About Hypermobility and Management Strategies
The body of hypermobility research is growing, particularly around pain, proprioception, and autonomic nervous system involvement. Current hypermobility research highlights the importance of active stabilization, graded movement, and avoiding overly aggressive passive treatments.
Research also supports individualized care plans and interdisciplinary approaches. When reviewing hypermobility research, it’s important to remember that what works for one hypermobile person may not work for another—flexibility in care is key. We have compiled a list of articles that the Ehlers-Danlos Society uses for educational trainings that patients may find helpful.
How Chiropractic Care Can Be An Effective Management Strategy
When adapted correctly, chiropractic care can play a supportive role in hypermobility management. Gentle, low-force techniques can help improve joint awareness, reduce protective muscle tension, and support nervous system regulation without overstressing connective tissue.
Chiropractic approaches that focus on stabilization rather than “cracking” joints are especially helpful for people with hypermobile Ehlers Danlos and HSD. This is where provider training and experience truly matter.
Chiropractic Care That Is Focused On Hypermobile Patients
Not all chiropractic care is created equal. Chiropractic care for hypermobile patients should prioritize safety, consent, and nervous system awareness. This includes:
Avoiding high-velocity techniques when inappropriate or in regions that are less stable
Supporting proprioception and postural control through movement and taping
Integrating breathwork and regulation strategies
For people with hypermobility, chiropractic care should feel grounding—not destabilizing. When done well, it becomes a collaborative part of long-term hypermobility management rather than a quick fix.
Book an Appointment with Dr. Savannah
If you’re newly diagnosed—or suspect hypermobility may be part of your story—working with a provider who truly understands hypermobility matters. Dr. Savannah offers chiropractic care specifically tailored to hypermobile patients, including those with Hypermobility Spectrum Disorder and hypermobile Ehlers Danlos.
Care is gentle, trauma-informed, and focused on long-term stability and regulation.
👉 Book an appointment with Dr. Savannah today and start building a care plan that supports your whole body.
-Dr. Savannah
FAQs About HSD and hEDS
What is the difference between HSD and hEDS?
HSD is diagnosed when symptomatic hypermobility is present without meeting full criteria for hypermobile Ehlers Danlos. Both conditions can cause significant pain and require similar hypermobility management strategies. The diagnostic criteria will be changing in 2027 for both disorders and will focus on if a patient is symptomatic of asymptomatic rather than differentiating between the two.
Is it safe to see any chiropractor as a hypermobile person?
Not necessarily. Hypermobile patients should seek chiropractic providers who understand hypermobility and avoid one-size-fits-all techniques. Experience with Ehlers Danlos and joint instability is crucial for safety and that is true of any healthcare provider you may be seeking with hypermobility.
Should I seek formal diagnosis and where do I go?
A formal diagnosis can be helpful for validation, accommodations, and care planning. Rheumatologists and geneticists are often involved, but primary care providers familiar with hypermobility research can also guide next steps or provide diagnosis. Using trusted hypermobility resources can help you find appropriate clinicians.
Is there treatment for hypermobility?
There is no cure, but effective hypermobility management exists. Treatment focuses on stabilization, nervous system regulation, movement education, and supportive care like chiropractic, physical therapy, and lifestyle adaptations. With the right support, many people experience meaningful improvement in function and quality of life.